Dizziness, Balance and Vertigo
Dizziness and Balance
At Dallas Ear Institute, our team of otoneurologists and audiologists work to diagnose, treat, and manage balance disorders related to the vestibular and central systems. However, not all dizziness symptoms and balance disorders are ear related. This is why we strongly suggest you review your balance and dizziness symptoms with your primary care physician or family doctor prior to scheduling an appointment with an ear specialist. Typically your primary physician will be able to diagnose and treat common balance disorders or refer you to the appropriate specialist if needed.
Diagnostic Testing for Balance Disorders
General Balance Information
Usually taken for granted, the sense of balance is an automatic body function until insult or injury to the balance system occurs. A balance disorder is a disturbance which causes sensations of being unsteady, dizzy, spinning, disorientation, tipping over, or floating, even though you are standing still or lying down.
Everyone experiences dizziness at least once at some point in their lives. Single instances of balance disturbances can be attributed to dehydration, overexertion, excessive alcohol intake, moving from a bending to a standing position too quickly, following a roller coaster ride, etc. However, when dizziness, imbalance, or falls become frequent occurrences an underlying condition may be the cause.
Our sense of balance is controlled by three systems: the vestibular system (inner ears), the visual system (eyes), and the proprioceptive system (bones and joints). Sensory input from these three systems is integrated and processed by the brainstem and brain (central system). In return, feedback is sent from the brain to the eyes and body to help maintain visual focus, correct posture and balance. A disruption in any of these four areas can cause a balance disorder as well as other associated symptoms.
At Dallas Ear Institute, our team of otoneurologists and audiologists work to diagnose, treat, and manage balance disorders related to the vestibular and central systems.
What Is Dizziness?
Dizziness is an umbrella term used to describe a group of sensations typically associated with unsteadiness or whirling. Using the term “dizziness” has no specific medical meaning; therefore, your doctor may ask you to describe the sensations you feel to group you in one or more of the following conditions:
Vertigo - The false sense of your body or your environment moving or spinning when no movement is truly taking place. Vertigo is usually a sign of an ear related disorder and accounts for 50% of dizziness complaints.
Disequilibrium - A problem with keeping balanced or the sensation of being unsteady on your feet.
Lightheadedness (presyncope) - The sensation of feeling like you're about to faint. This sensation is almost always brought on by a reduced amount of blood to the brain. Commonly felt when standing up too quickly, hyperventilating, reduction in blood pressure, or by being dehydrated.
Anxiety - People who are scared, worried, depressed, or afraid of open spaces may use "dizzy" to mean frightened, depressed, or anxious.
What Does Vertigo Mean?
Vertigo is a form of dizziness which is defined as the false perception of movement. Most of the time vertigo is described as a spinning sensation similar to that of spinning on a merry-go-round. Vertigo is usually indicative of a vestibular dysfunction and accounts for 50% of all dizziness complaints.
Vertigo - The false sense of your body or your environment moving or spinning when no movement is truly taking place. Vertigo is usually a sign of an ear related disorder and accounts for 50% of dizziness complaints.
Disequilibrium - A problem with keeping balanced or the sensation of being unsteady on your feet.
Lightheadedness (presyncope) - The sensation of feeling like you're about to faint. This sensation is almost always brought on by a reduced amount of blood to the brain. Commonly felt when standing up too quickly, hyperventilating, reduction in blood pressure, or by being dehydrated.
Anxiety - People who are scared, worried, depressed, or afraid of open spaces may use "dizzy" to mean frightened, depressed, or anxious.
How Long Does Vertigo Last?
The length of vertigo attacks can range from a fleeting second to multiple days. How long a vertigo attack lasts is determined by what is causing the vertigo in the first place. For example: patients experiencing Benign Paroxysmal Positional Vertigo (BPPV) -the most common reason people experience vertigo- only notice vertigo lasting a few seconds at a time after making a head or body movement. In contrast, patients suffering from vestibular neuritis can notice symptoms lasting for several hours to days at a time.
TIP: Keep a log of your symptoms, the duration, and any associated triggers and share this information with your doctor. How long and how often your vertigo is experienced is a very helpful tool in quickly diagnosing and treating your balance disorder.
What Is the Vestibular System
The medical term for all of the parts of the inner ear involved with balance is the vestibular system. The vestibular system is responsible for sensing changes in head movement which is imperative for maintaining postural control of the body as well as being able to keep the eyes focused on objects during movement.
The balance receptors in the vestibular system provide incredibly precise head motion information which is used by the central vestibular pathways to control the eye and body reflexes.
TIP: Keep a log of your symptoms, the duration, and any associated triggers and share this information with your doctor. How long and how often your vertigo is experienced is a very helpful tool in quickly diagnosing and treating your balance disorder.
How Does the Vestibular System Work?
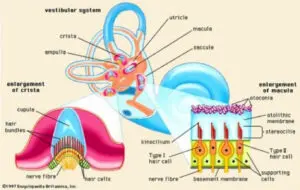
The vestibular system is a labyrinth within in each temporal bone (one for each ear). Each labyrinth is split into two sections: the semicircular canals and the otolithic organs.
The semicircular canals are three fluid-filled loops arranged roughly at right angles to each other. Each semicircular canal has a plump base, which contains a raindrop-shaped structure filled with a gel-like substance. This structure, called the cupula, sits on top of a cluster of sensory cells, called hair bundles. The hair bundles have long threadlike extensions, called stereocilia, that extend into the gel. When the head moves, fluid inside the semicircular canal moves. This motion causes the cupula to bend and the stereocilia within it to tilt to one side. The tilting action creates a signal that travels to the brain to tell it the movement and position of your head.
Between the semicircular canals and the cochlea lie the otolithic organs, which are two fluid-filled pouches called the utricle and the saccule. These organs tell the brain when our body is moving in a straight line, such as when we stand up or ride in a car or on a bike. They also tell the brain the position of our head with respect to gravity, such as whether we are sitting up, leaning back, or lying down.
Like the semicircular canals, the utricle and the saccule have sensory hair bundles. These hair bundles line the bottom of each pouch, and their stereocilia extend into an overlying gel-like layer. On top of the gel are tiny grains made of calcium carbonate called otoconia. (Otoconia are often referred to as “ear crystals”.) When you tilt your head, gravity pulls on the grains, which then move the stereocilia. As with the semicircular canals, this movement creates a signal that tells the brain the head's position.
The balance receptors in the vestibular system provide incredibly precise head motion information which is used by the central vestibular pathways to control the eye and body reflexes.
TIP: Keep a log of your symptoms, the duration, and any associated triggers and share this information with your doctor. How long and how often your vertigo is experienced is a very helpful tool in quickly diagnosing and treating your balance disorder.
Symptoms of a Vestibular Dysfunction?
Persons suffering from vestibular balance disorders may report one or more of the following symptoms:
- Ear fullness (One or both ears feel stopped up or clogged)
- Ear pain
- Falling or feeling as if you are going to fall
- Head movements initiate symptoms (Rolling over in bed, looking up or down, turning head, bending over)
- Hearing loss (Fluctuating or stable)
- Loss of hearing clarity or speech understanding
- Loud sounds initiate vertigo symptoms
- Nausea and vomiting
- Ringing, buzzing, or humming in the ears (Tinnitus)
- Sneezing, blowing nose, or straining initiates symptoms.
- Spinning (Vertigo)
Symptoms may come and go or be constant. It is important to note how often and for how long you experience each symptom. This information can help your doctor accurately identify the source of your balance disorder.
Causes of Vestibular Dysfunction?
A vestibular or ear related balance disorder may be caused by viral or bacterial infections in the ear, head injuries, tumors, congenital disorders, hereditary disorders, or blood circulation disorders that affect the inner ear or brain. Many balance disorders can begin suddenly and with no obvious cause.
- Acoustic neuroma
- Allergies
- Autoimmune inner ear disease
- Benign paroxysmal positional vertigo (BPPV)
- Cholesteatoma
- Endolymphatic hydrops / Meniere’s Disease
- Enlarged Vestibular Aqueduct Syndrome
- Head trauma
- Vestibular migraines
- Labrynthitis
- Mal de Debarquement
- Middle ear pressure changes -
- Otitis media
- Otosclerosis
- Ototoxicity
- Perilymph Fistula
- Superior Semicircular Canal Dehiscence (SSCD)
- Temporal bone trauma
- Vestibular neuritis
Common Types of Vestibular Dysfunctions?
There are more than a dozen different balance disorders. Some of the most common are:
Benign Paroxysmal Positional Vertigo (BPPV) or positional vertigo is a brief, intense episode of vertigo that occurs because of a specific change in the position of the head. If you have BPPV, you might feel as if you're spinning when you look for an object on a high or low shelf or turn your head to look over your shoulder (such as when you back your car up). You may also experience BPPV when you roll over in bed. BPPV is caused when otoconia (“ear crystals”) become dislodged and tumble from the utricle into one of the semicircular canals and weigh on the cupula. The cupula can't tilt properly and sends conflicting messages to the brain about the position of the head, causing vertigo. BPPV
Labyrinthitis is an infection or inflammation of the inner ear that causes dizziness and loss of balance. It is frequently associated with an upper respiratory infection such as the flu.
Ménière's Disease is associated with a change in fluid volume within parts of the labyrinth. Ménière's disease causes episodes of vertigo, irregular hearing loss, tinnitus (a ringing or buzzing in the ear), and a feeling of fullness in the ear. The cause of this disease is unknown. For more information, read the NIDCD fact sheet Ménière's Disease.
Vestibular Neuronitis is an inflammation of the vestibular nerve and may be caused by a virus. Its primary symptom is vertigo.
Perilymph Fistula is a leakage of inner ear fluid into the middle ear. It can occur after a head injury, drastic changes in atmospheric pressure (such as scuba diving or skydiving), physical exertion, ear surgery, or chronic ear infections. Its most notable symptom, besides dizziness and nausea, is unsteadiness when walking or standing that increases with activity and decreases with rest. Some babies may be born with perilymph fistula, usually in association with hearing loss that is present at birth.
Mal de Debarquement Syndrome (MdDS) is a balance disorder in which you feel as if you're continuously rocking or bobbing. It generally happens after an ocean cruise or other sea travel. Usually, the symptoms will go away in a matter of hours or days after you reach land. However, severe cases can last months or even years.
sometimes may result from a head injury, sedentary lifestyle, or from getting older.
The Prevalence of Vestibular Dysfunction?
One study estimates that as many as 35% of adults aged 40 years or older in the United States—approximately 69 million Americans—have experienced some form of vestibular dysfunction.1
According to the National Institute on Deafness and Other Communication Disorders (NIDCD), an additional 4% (8 million) of American adults report a
chronic problem with balance, while an additional 1.1% (2.4 million) report a chronic problem with dizziness alone.2
Eighty percent of people aged 65 years and older have experienced dizziness.3
BPPV, the most common vestibular disorder, is the cause of approximately 50% of dizziness in older people.4
Overall, vestibular problems account for 1/3 of all dizziness and vertigo symptoms reported to health care professionals.5
If My Balance Problem Is Not Ear Related, Then What Is It?
Some non-ear related causes of balance dysfunction:
- Agoraphobia
- Anemia
- Aneurysm
- Brainstem disease
- Cerebrovascular disease
- Cervical or spine disorder
- Chiari Malformation
- Dehydration
- Demyelinating disease
- Diabetes
- Drug reactions
- Heat exhaustion
- Hyperventilation
- Lung disease
- Malnutrition
- Migraine
- Neurodegenerative disease
- Neuropathy
- Panic disorders
- Persistent postural perceptual dizziness
- Poor blood circulation or volume
- Pregnancy
- Psychiatric disorders
- Sedentary lifestyle
- Sleep apnea
- Vascular compression
- Visual disorder
How Do I Get Help for My Balance Disorder?
First, schedule an appointment with your family doctor or your primary care provider (PCP). These are physicians, physician assistants, and nurse practitioners who see patients with acute and chronic illnesses, have the widest understanding of your overall health, and are usually able to diagnose and manage your balance disorder.
Your family doctor or PCP may also refer you to a specialist they believe will be able to more appropriately diagnose and manage your symptoms such specialists in ear, nose, and throat conditions (ENT/otolaryngologist), hearing and balance conditions (audiologist), cardiovascular conditions (cardiologist), brain and nervous system conditions (neurologist), mental health disorders (psychiatrists and psychologists), physical medicine and rehabilitation (PM&R/physiatrists), and physical therapists (PT).
What Tests Are Used to Diagnose Balance Disorders
To evaluate a vestibular or ear related balance disorder, your family doctor or PCP may suggest you see an otolaryngologist (a physician and surgeon who specializes in the ear, nose, and throat), an otoneurologist (a physician and surgeon who specializes in disorders of the ear and skull base tumors) or an audiologist (a clinical doctor who specializes in diagnosing and rehabilitating hearing and balance disorders). These specialists use the following tests to assess the cause and extent of the balance disturbance depending on your symptoms and health status.
Some of the tests include:
- Blood pressure and heart rate tests
- Electrocochleography (ECOG or ECochG)
- Hearing examination
- Imaging studies of your head and brain (MRI or CT)
- Posturography
- Urinalysis
- Vestibular evoked myogenic potential (VEMP)
- Videonystagmography (VNG or ENG)
How Are Balance Disorders Treated?
Your treatment options will depend on the cause of your balance disorder, severity of symptoms and disability, and medical history. Balance disorder treatments range from lifestyle changes, diet modifications, medication modifications, physical therapy, occupational therapy, and in some cases surgery.
In most cases, vertigo is easily treatable or the body is able to naturally compensate for the vestibular disorder. This causes symptoms to become decreased or eliminated on their own. However, some people with a balance disorder may not be able to fully relieve their dizziness and will have to develop ways to cope with it on a daily basis. A vestibular rehabilitation therapist can help by developing an individualized treatment plan that combines head, body, and eye exercises to decrease dizziness and nausea.
To reduce your risk of injury from dizziness, avoid walking in the dark. You should also wear low-heeled shoes or walking shoes outdoors and use a cane or walker if necessary. If you have handrails in the home, inspect them periodically to make sure they are safe and secure. Modifications to bathroom fixtures can make them safer. Conditions at work may need to be modified or restricted, at least temporarily. Driving a car may be especially hazardous. Ask your doctor's opinion about whether it's safe for you to drive.
At Home Exercises
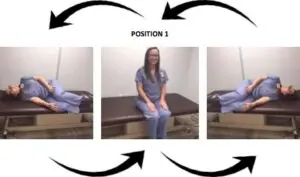
Brandt-Daroff Exercise
To complete ONE CYCLE:
1) Begin by sitting upright on a bed. 2) Quickly lie down onto one side while also turning your head to a 45 degree angle as you lower yourself onto the bed. Make sure that you are looking up at the ceiling. Take no more than 1-2 seconds to go from sitting to laying. 3) Keep your head looking up at a 45 degree angle as you hold this laying position for 30 seconds, or until dizziness subsides. 4) Return to an upright position and face forward. Stay in this position for 30 seconds. 5) Now lie down onto the opposite side. Again, you should be turning your head up to a 45 degree angle to look up at the ceiling as you lie down. It should take no more than 1-2 seconds to go from sitting to the laying position. 6) Remain lying on this side for 30 seconds, or until dizziness subsides. 7) Return to an upright position and face forward. Stay in this position for 30 seconds. THIS IS ONE CYCLE. REPEAT CYCLE FIVE TIMES TO MAKE ONE SET. REPEAT THREE SETS PER DAY FOR 14 DAYS.
What is BPPV?
BPPV or Benign Paroxysmal Positional Vertigo is one of the most common disorders of the inner ear that results in vertigo. It is due to particles that have collected in the fluid filled inner ear. These particles float in the fluid and will occasionally touch a sensitive area resulting in the sensation of vertigo. The name of this disorder is derived from the fact that BPPV is benign (not life threatening), paroxysmal (dizziness occurs suddenly and is generally brief) and it is positional (dizziness occurs with particular head positions).
What are the symptoms of BPPV?
The symptoms can vary in each person but are generally brought on by movement or position changes of the head. Laying back, tilting the head backwards or rolling over in bed are common “problem” motions. Although many people feel normal when not in a stimulating position, some do have a sensation of imbalance. The symptoms can last for days, months or occasionally forever. In some the dizziness can come back after it resolves completely.
What causes BPPV?
In most people, BPPV occurs for no apparent reason (idiopathic). In a small group of people it occurs after a head injury.
How is the diagnosis made?
Your doctor will make the diagnosis based on your symptoms, physical examination and the results of your hearing and balance tests. Occasionally other tests may be required.
How is BPPV treated?
1. The particle repositioning maneuver can be performed in the office by your physician. In this maneuver, the particles are placed in an unimportant part of the inner ear. You will be asked to lie on your back with your head turned towards the “bad” side which will make you temporarily dizzy. Then your head (along with your body) is rotated around towards the “good” ear. To increase the success of the maneuver, you will be asked to: a. Sleep upright as best you can for 48 hours. Use of a recliner or pillows is beneficial. b. For one week, avoid the movements that have caused dizziness such as bending over, moving your head quickly or laying on the bad ear. c. A soft cervical collar can be used as a reminder for you to avoid quick motions and particular positions.
Download Brandt-Daroff Exercises
Cawthorne's Exercises
These exercises should be carried out for 4 minutes, 10 times per day. You can expect dizziness when beginning these exercises and you will find this lessen over time with repetition.
1. Eye Exercises
A. Slowly look up and then down, then quickly 20 times. B. Slowly look from side to side, then quickly 20 times. (Try to focus on an object at the end of each head turn.)
2. Head Exercises:
A. With eyes open, slowly bend forward and then backwards, then quickly 20 times. B. Slowly turn head from one side to the other, then quickly 20 times. (As dizziness lessens, these head exercises should be done with eyes closed.)
3. Sitting/Bending:
A. While sitting, slowly shrug your shoulders 20 times. B. Turn shoulders to the right, then to the left 20 times. C. Bend forward and pick up objects from the ground and sit up 20 times.
4. Standing:
A. Change from a sitting to standing position, and sitting again 20 times. (Do this initially with eyes open. As balance improves, do this with eyes closed (but only if you have a partner to help you.) B. Throw a rubber ball (or similar object) from hand to hand above eye level.
Citations
- Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults. Arch Intern Med. 2009;169(10): 938-944.
- National Institute on Deafness and Other Communication Disorders (NIDCD). Strategic Plan (FY 2006-2008). Available at: www.nidcd.nih.gov/StaticResources/about/plans/strategic/strategic06-08.pdf. Accessed May 20, 2010.
- Ator GA. Vertigo—Evaluation and Treatment in the Elderly.
- Fife TD, Iverson DJ, Lempert T, Furman JM, Baloh RW, Tusa RJ, Hain TC, Herdman S, Morrow MJ, Gronseth GS. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurol. 2008;70:2067–2074.
- Neuhauser HK, Radtke A, von Brevern M et al. Burden of dizziness and vertigo in the community. Arch Intern Med. 2008;168(19):2118–2124.